What is Dry Needling
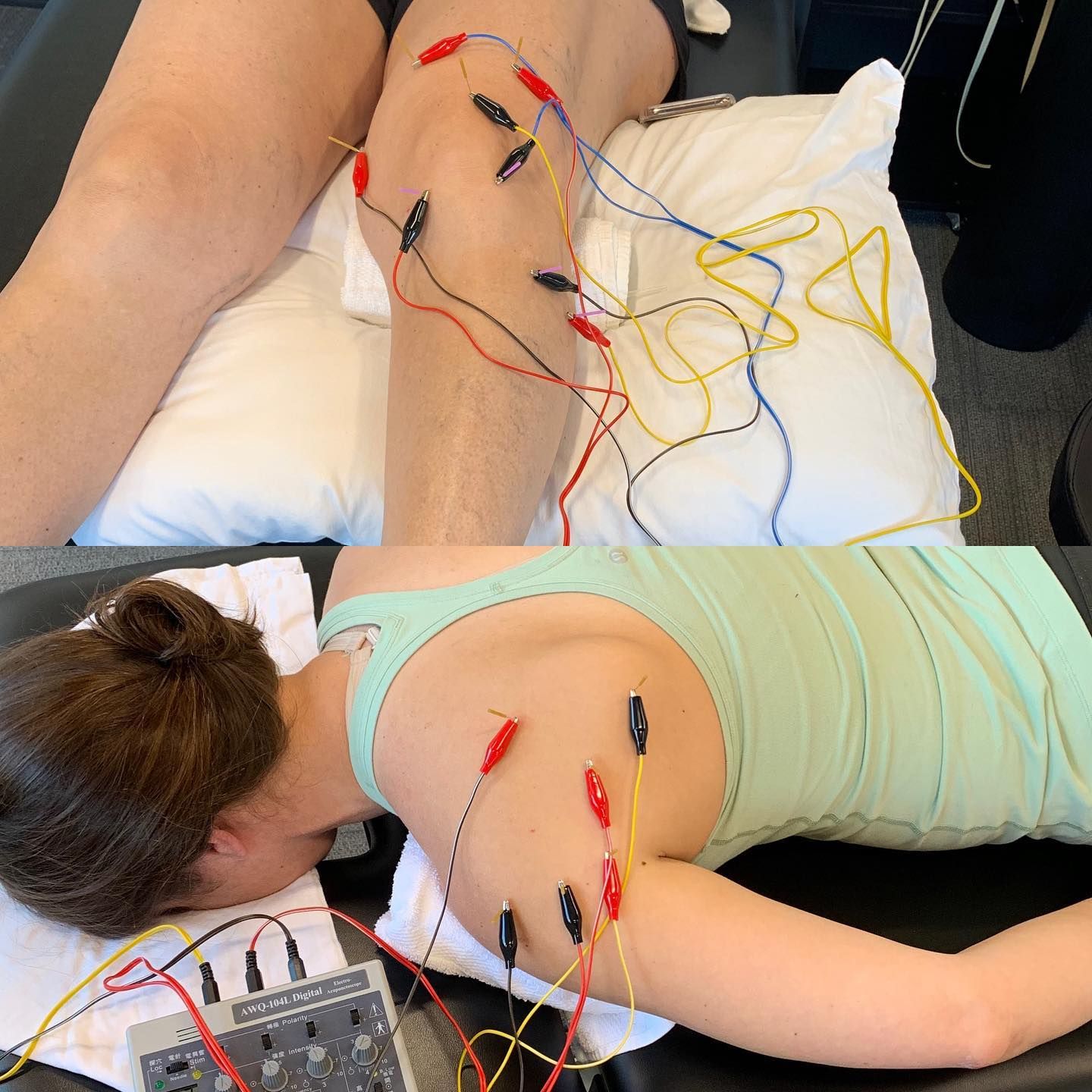
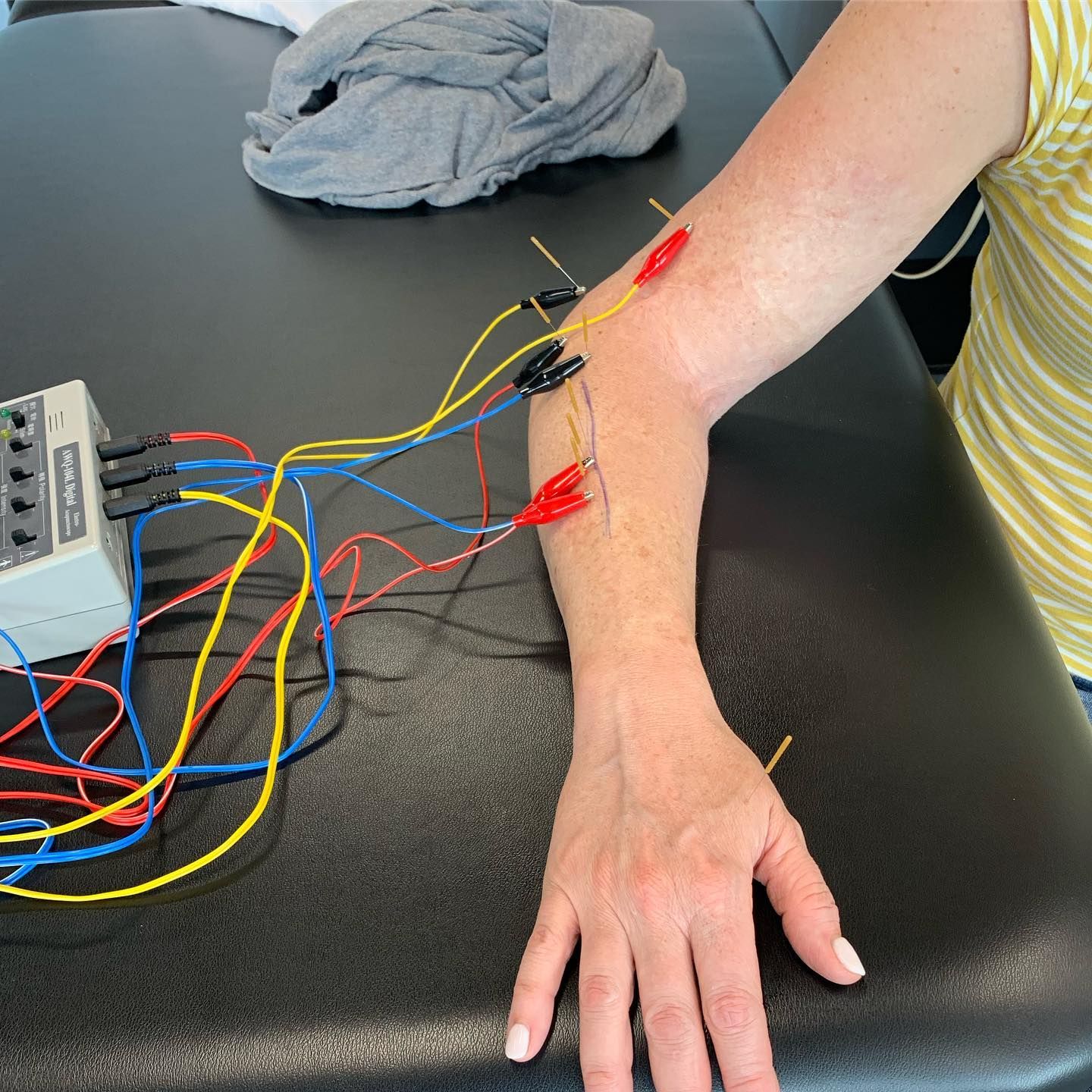
State of Idaho Definition: Idaho Code 54-2203 “Dry needling” means a skilled intervention performed by a physical therapist that uses a thin filiform needle to penetrate the skin and stimulate underlying neural, muscular and connective tissues for the evaluation and management of neuromusculoskeletal conditions, pain and movement impairments.
Dry Needling is a form of therapy in which fine needles are inserted into targeted areas and/or myofascial trigger points (painful knots in muscles), tendons, ligaments, or near nerves to stimulate a healing response in painful musculoskeletal conditions. Dry needling is not acupuncture or Oriental Medicine; that is, it does not have the purpose of altering the flow of energy (“Qi”) along traditional Chinese meridians for the treatment of diseases. In fact, dry needling is a modern, science-based intervention for the treatment of pain and dysfunction in musculoskeletal conditions such as neck pain, shoulder impingement, tennis elbow, carpal tunnel syndrome, headaches, knee pain, shin splints, plantar fasciitis, low back pain, ect.
Is all Dry Needling the same?
In short, No. There are many companies that offer Dry Needling Certifications that only focus on Trigger Point Dry Needling, that is finding a trigger point or “hot spot”, taking a dry needle and inserting the needle into that trigger point several times (often called ‘pistoning’) trying to elicit a localized twitch response. This is only one technique that often only provides short term relief and the evidence surrounding the use of MTrP’s is lacking when it comes to sustained long term results.
How are we Different?
All our Doctor’s of Physical Therapy have trained with Dr. James Dunning, DPT, MSc (Manip Ther), MAACP (UK), FAAOMPT, Dip. Osteopractic and/or Dr. Raymond Butts, PhD, DPT, MSc (NeuroSci), MAACP (UK), Cert. DN, Dip. Osteopractic and are certified by the Dry Needling Institute. We utilize ALL relevant research to properly treat your specific condition and we can point to literature supporting our chosen needle placement, utilization of MTrP’s, the number of needles, duration the needles are left in-situ, the use of electrical current and use of other manual therapy/spinal manipulation techniques in conjunction with Dry Needling. A list of relevant research is provided at the bottom of this page.
IS Dry Needling Safe?
Dry needling is generally considered to be a safe and effective treatment when performed by a trained and qualified healthcare professional. As with any medical procedure, there are some potential risks and side effects associated with dry needling. These may include:
• Bruising or bleeding at the needle insertion site
• Mild pain or discomfort during or after the treatment
• Temporary worsening of symptoms
• Fainting or dizziness
• Infection
• Nerve damage
Most of these side effects are rare and can be effectively managed by the healthcare professional performing the treatment. It is important to inform your healthcare provider about any medical conditions you have or medications you are taking before undergoing dry needling, as this may affect your suitability for the treatment.
What does the Literature Say?
These journal articles include multi-center randomized controlled trials, clinical guidelines, literature reviews, case series & case reports.
11. Cavitation Sounds During Cervicothoracic Spinal Manipulation (Dunning et al, 2017)